During IVF, you may hear terms like “Grade A embryo,” “blastocyst quality,” or “ICM and TE grading.” Many couples feel anxious or confused trying to decode what these scientific labels mean — and whether their embryo is “good enough.”
In reality, embryo grading is simply a tool that embryologists use to understand how an embryo is developing. It helps predict the likelihood of implantation, but it’s not a guarantee of success or failure.
At Renew Healthcare, we believe in educating couples so they can make informed decisions during their IVF journey. Understanding embryo grading helps reduce stress and gives you clarity about what’s happening in the lab.
Embryo grading is a standardized way of evaluating how embryos grow and develop. The goal is to select the embryo with the highest potential for implantation and a healthy pregnancy.
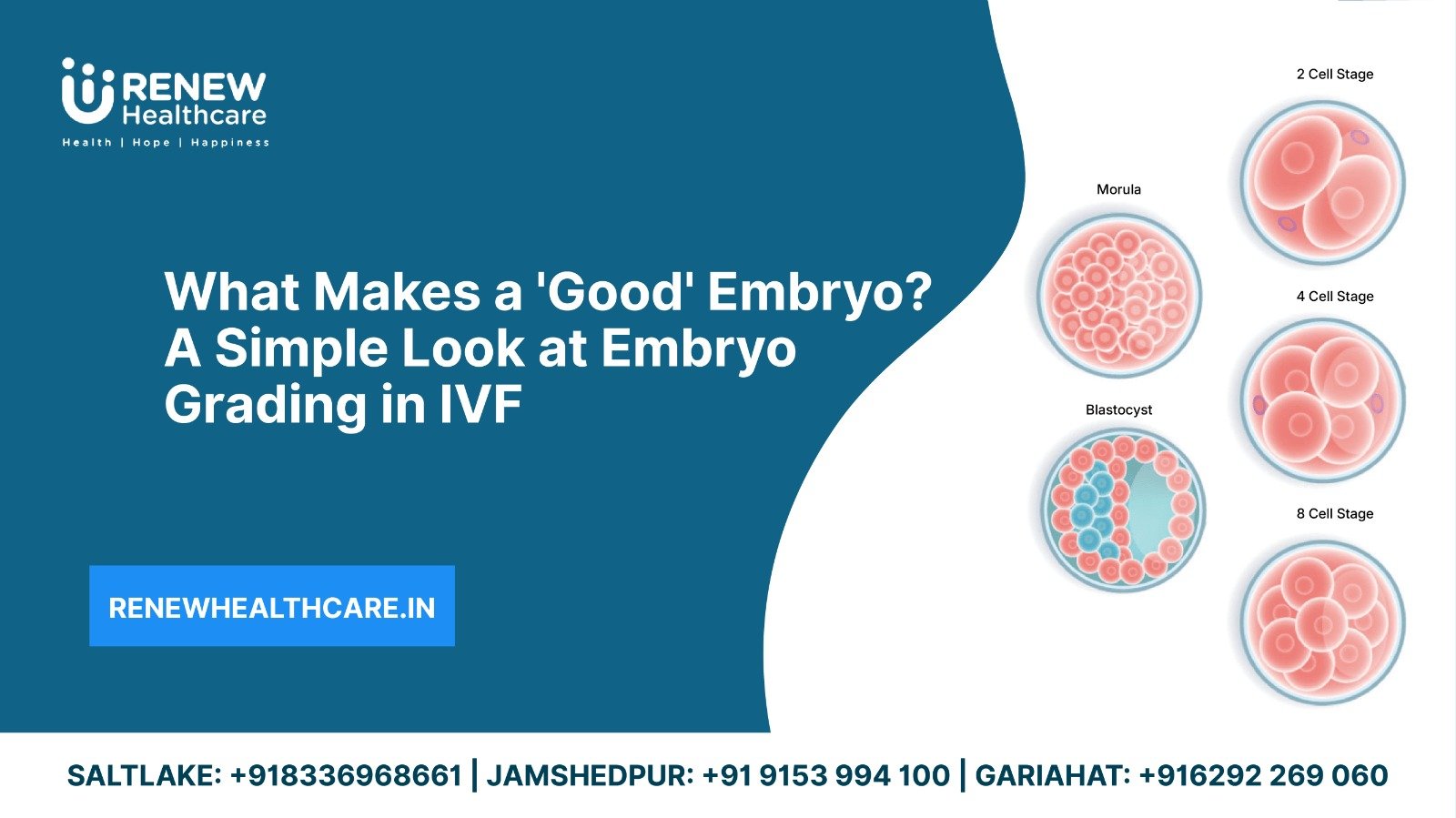
Embryo development is assessed at different stages, primarily:
Each stage has a different grading system.
On Day 3, the embryo typically has 6–8 cells. Embryologists check:
A high-quality Day 3 embryo has:
However, Day 3 grading gives limited information since genetics are not visible at this stage.
Day 5 blastocysts are more advanced and provide better information about future implantation. These have two main structures:
Example of blastocyst grade:
4AA = expanded blastocyst, excellent ICM, excellent TE
3BC = full blastocyst, good ICM, lower TE quality
1AB = early blastocyst, excellent ICM, good TE
Higher grades (AA, AB, BA) often have better chances of implantation — but even BC or CB embryos can lead to healthy babies.
PGT-A (Preimplantation Genetic Testing for Aneuploidy) checks embryos for genetic abnormalities. Even a perfect AA embryo can have an abnormal chromosome number, so visual grading alone isn’t enough.
PGT-A helps:
Couples with repeated failures or advanced maternal age often benefit most.
MitoScore measures mitochondrial activity in the embryo.
This test is an additional tool to help select embryos with the best developmental potential.
Embryo quality is influenced by several biological and environmental factors, and understanding these helps couples appreciate why some embryos develop stronger than others. One of the biggest determinants is egg quality, which naturally declines with age. As women age, the number of healthy chromosomes within the eggs decreases, increasing the chance of poor-quality embryos or abnormal development. Conditions like PCOS, endometriosis, or hormonal imbalances can also affect the health of the eggs released during an IVF cycle.
Likewise, sperm health plays a major role in embryo development. Poor sperm motility, morphology, or DNA fragmentation can contribute to abnormalities in early cell division. Even when ICSI (Intracytoplasmic Sperm Injection) is used, sperm DNA quality still influences embryo growth, blastocyst formation, and implantation potential.
Beyond egg and sperm factors, the IVF laboratory environment is equally essential. Embryos are extremely delicate and require precise conditions for growth — including stable temperature, optimal culture media, perfect pH, and low exposure to environmental toxins. Advanced labs with high-quality incubators and air filtration systems help embryos develop in an environment that closely mimics natural conditions.
Finally, genetics play a powerful role. Some embryos may appear perfect under the microscope but may have chromosomal abnormalities, which can reduce the chances of implantation or lead to miscarriage. Tests like PGT-A (Preimplantation Genetic Testing for Aneuploidy) help determine whether embryos are genetically normal. Technologies like MitoScore also help assess the mitochondrial activity of embryos, giving doctors deeper insight into embryo viability and predicting which embryos may have stronger implantation potential.
Embryo grading is an important tool in IVF, but it’s not the final word on whether an embryo will result in a healthy pregnancy. Embryo grading is essentially a visual assessment—embryologists look at how evenly the cells divide, how compact or expanded the blastocyst appears, and how strong the inner cell mass and trophectoderm look. While this provides useful guidance, it does not assess the embryo’s genetic health or implantation behavior.
Many couples are surprised to learn that even lower-grade embryos can lead to perfectly healthy pregnancies and babies. A “B” or “C” grade embryo simply means the appearance isn’t ideal, not that the embryo is defective. Some embryos develop slowly but catch up after implantation. Others may look imperfect in the lab yet be genetically normal and capable of forming a strong pregnancy.
On the other hand, even a “top-grade” embryo may fail to implant if it carries chromosomal abnormalities that grading cannot detect. This is why doctors often emphasize that grading is only one part of the bigger picture. Factors such as uterine lining health, hormonal balance, immune function, and overall embryo genetics also determine outcomes.
In short, grading helps guide the selection process, but it does not guarantee success or failure. It is simply one piece of information used to choose the most promising embryo for transfer.
At Renew Healthcare, embryo development is supported by state-of-the-art technology and the expertise of highly skilled embryologists. Our IVF lab is equipped with advanced incubators that maintain stable temperature, humidity, and CO₂ levels — ensuring embryos develop in the most natural and protective environment possible. Every step of the process is carefully monitored to reduce environmental stress and promote optimal growth from fertilization to the blastocyst stage.
Our embryologists follow internationally recognized grading guidelines and use high-resolution imaging systems to evaluate embryos with precision. This includes assessing the Inner Cell Mass (ICM), which becomes the baby, and the Trophectoderm (TE), which forms the placenta. By carefully observing cell division patterns and blastocyst expansion, our team identifies which embryos have the highest potential for implantation.
Renew Healthcare also integrates advanced tools such as PGT-A for genetic screening and MitoScore analysis to further enhance embryo selection accuracy. These technologies help ensure that the healthiest, most viable embryos are chosen for transfer, especially for couples with previous IVF failures, advanced maternal age, or recurrent miscarriages.
With a combination of cutting-edge lab technology, strict quality control, and deep clinical expertise, Renew Healthcare provides couples with the highest standard of embryo assessment and care — giving every embryo the best possible chance to become a healthy baby.
A “good embryo” is not defined by a single grade or number. Embryo grading helps embryologists understand development — but it doesn’t define your chances of becoming a parent.
Many lower-grade embryos become healthy babies, and higher-grade embryos sometimes don’t implant.
What truly matters is a combination of embryo quality, genetic screening, lab conditions, and your overall reproductive health.
At Renew Healthcare, we offer advanced IVF techniques, expert embryology, and personalized support to help you build your family with confidence.
👉 Book your IVF consultation today at Renew Healthcare.
An IVF cycle ending in a negative result is emotionally painful, frustrating, and confusing — but it is not the...
The IVF journey can be one of the most emotionally intense experiences a couple faces. From hormone injections and medical...
Planning a pregnancy is one of the most meaningful steps in your life — but the journey doesn’t begin only...
Male fertility is not the subject of much discussion. Even when it is being discussed, the focus is more on...
Many couples mistakenly assume that they can easily have another child once they have had a successful pregnancy. However, at...
Male fertility is closely associated with the health of sperm. A healthy sperm count and strong motility are essential for...
IVF fertility treatment is difficult and emotionally draining. It is a time that is often marked by anxiety, hope, and...
Low sperm count is a condition that, as the name suggests, is marked by fewer sperm. When the male semen...
Infertility is a condition that affects both men and women. In women, infertility is described as the inability of a...
Meet Priyanka, a busy marketing professional. Lately, her periods have become heavy and unpredictable. Cramping disrupts her workday, and she’s...
